Are Three Brain Imaging Techniques Better than One?
New NIH grants will allow SDSU psychologist Ralph-Axel Mller to explore the autistic brain using fMRI, EEG, and MEG brain imaging technologies in tandem.
Many recent imaging studies have shown that in children with autism, different parts of the brain do not connect with each other in typical ways. Initially, most researchers thought that the autistic brain has fewer connections between key regions. The most recent studies, however, point to an opposite conclusion: The brains of people with autism exhibit overconnectivity.
To date, almost all studies of autism in children have used a single imaging technique to explore connectivity. None has been able to capture a robust picture of the brain abnormalities associated with autism—until now.
Two new grants from the National Institute of Mental Health (NIMH) will allow San Diego State University Psychology Professor Ralph-Axel Müller to combine three imaging techniques and harness the best of each one in his study of autism.
Techniques in tandem
Although the term “brain imaging” gets thrown around a lot when describing the latest advances in neuroscience and psychology, there are dozens of different brain imaging techniques. Each gives scientists a different view of the inner workings of the brain, and each comes with its own strengths and limitations.
For example, the frequently cited technique of fMRI, or functional magnetic resonance imaging, measures blood flow in different areas of the brain at specific snapshots in time, based on the knowledge that increased blood flow indicates increased activity of nerve cells in that area of the brain. The technique is powerful, but has limitations when it comes to detecting dynamic changes in brain activity that occur very fast, within milliseconds.
EEG (electroencephalography), a much older technique, is actually better at detecting such dynamic changes, although it cannot pinpoint exactly where in the brain the activity occurs. A powerful and more recent technique is MEG, or magnetoencephalography, which can detect dynamic changes in brain activity that happen within a few milliseconds.
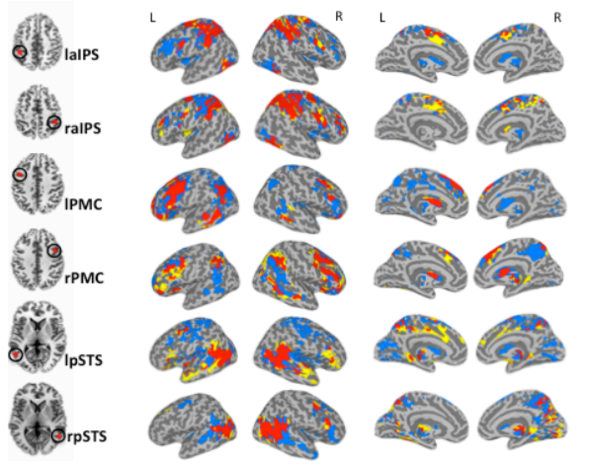
Müller looks for disorganized patterns of brain activity that could be responsible for some of the telltale characteristics of autism spectrum disorder, such as inattention to social cues and repetitive and obsessive behaviors. For example, last year, Müller and his colleagues discovered that in children with autism, connectivity was impaired between the cerebral cortex and the thalamus, a deep brain structure that is important for sensorimotor functions and attention.
With $3.7 million in new funding from NIH, Müller—together with collaborators Ksenija Marinkovic at SDSU and Thomas Liu at the University of California, San Diego—will apply fMRI, EEG, and MEG to study both autistic and non-autistic, or typically-developing, children and adolescents during a variety of tests, including language tests designed to tease out activity in various parts of the brain.
Defining the differences
One component of the project will concern the visual system. Previous research has shown that people with autism rely on their visual cortex more than typically- developing people during thought processes, for example, when making a semantic distinction, such as deciding whether a truck is a vehicle. Using the one-two punch of fMRI and MEG together, Müller and his team will be able to determine the dynamic processes in how brain regions work together to come up with a response, and how these processes differ in autism.
The study will also examine brain function during its resting state in order to identify abnormalities in brain network organization. The combined use of EEG and MEG, together with fMRI techniques that reveal brain anatomy, will produce a much more complete picture of abnormal brain organization in autism.
Ultimately, Müller and his colleagues hope to identify biomarkers in the brain that can reliably indicate whether the participant falls on the autism spectrum.
“Autism is a brain-based disorder, but its diagnosis is still based entirely on behavioral observation,” Müller said. “This is inadequate. We need to find brain biomarkers for autism.”
Another goal of the researchers is to find brain biomarkers that can distinguish different subtypes of autism. It is generally suspected that the term “autism” actually covers several different disorders, each of which may be caused by different genetic and environmental risk factors. Eventually, brain biomarkers might be tied to genetic data, giving scientists a better understanding of the origins of autism, as well as new leads for treatment.
“For decades, research teams studying autism have specialized in one or another scientific technique, often without understanding well what other techniques can reveal. Our study combining several of the major imaging techniques will be one step toward a more comprehensive account of how the autistic brain differs from the typically developing one – and what may be done about it,” Müller said.



