Breaking Through the Blood-Brain Barrier
SDSU researchers have discovered a molecular process that helps bacteria trick the brains defenses.
The bacteria that sneak past the brain’s defenses to cause deadly bacterial meningitis are clever adversaries. Brandon Kim would know. The biology graduate student at San Diego State University investigates the molecular tricks bacteria use to convince their host that they are harmless and cause disease.
In a recent paper published in the Journal of Clinical Investigation, Kim and his lab mentor, SDSU biology professor Kelly Doran, describe their recent discovery that bacteria take advantage of a molecular warning signal and induce the brain’s cellular armor to temporarily break down, letting in the bacterial horde. Their discovery could have far-reaching implications for treating and preventing bacterial meningitis.
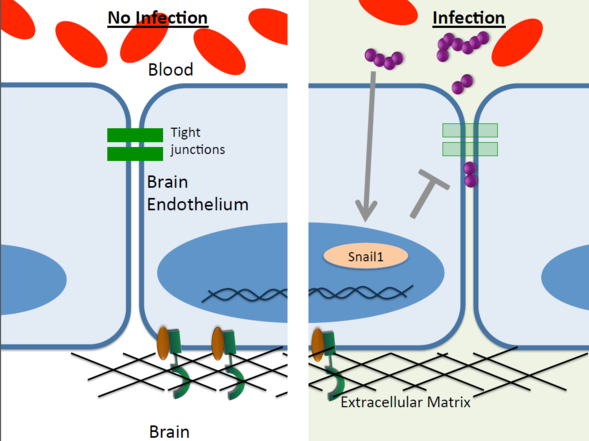
The blood-brain barrier is a thin network of blood vessels whose cells abut each other very closely, forming protein junctions too tight for bacteria and viruses to fit through. The barrier’s purpose is to prevent unwanted material from crossing over from the surrounding bloodstream into brain tissue.
Brick wall
“You can think of the blood-brain barrier as a brick wall,” explained Kim, who is completing his doctorate in Doran’s lab. “Each cell of the blood-brain barrier is a brick and these tight junctions are the mortar.”
Like castle guards, the cells that form this barrier can selectively let through nutrients and other “approved” molecules needed for normal brain function.
When bacteria or viruses do manage to slip past the blood-brain barrier and infect brain tissue, it can result in bacterial meningitis, a frequently deadly disease caused when the brain becomes dangerously inflamed.Using cell cultures, zebrafish and mice as models, Kim and Doran investigated how one type of bacteria, group B streptococcus, gets through the brain’s defenses.
By observing the bacteria’s advance at different points in time and analyzing which molecular processes were active at the time, the researchers discovered an interesting result. When receptors along the blood side of the blood-brain barrier detect group B strep, the system fires off a molecular “danger” signal. However, tied into this protective molecular signal is another, detrimental signal.
Stranger danger
When these blood-brain barrier cells fire off their danger signal, it not only induces the brain’s molecular “help” response but also induces a gene to produce a transcription factor protein known as Snail1 that contributes the breakdown of the barrier’s tight junctions. In doing so, the barrier unwittingly destroys its own integrity and permits the bacteria to enter the brain.
This study is the first to look at Snail1 in the context of meningitis. Previous research has described Snail1 as a factor of invasive cancer.
Understanding this process could allow scientists to develop therapeutics that temporarily control Snail1 expression and prevent the blood-brain barrier from acting on the hijacked self-destruct signal. Additionally, it might also allow researchers to harness the same process for good, designing drugs that tell the blood-brain barrier to let them through so they can fight various brain diseases.
“This finding will change the way that we view bacterial meningitis as a whole and may highlight new ways of treatment in the future,” Kim said.



